Consulo Indicium 6/18/18
Information for your Consideration…
A Diversionary Thought: I Thought I Was Useful – As most of my readers know, I moved into executive and managerial roles some time ago and when I’m asked by those I met the question – “So, where do you practice?” – my usual response is: “On United Airlines!” I answer that way because for the last 20+ years it seems that the clear majority of my time has been spent on planes traveling across the world. So, you can imagine my dismay when I recently picked up The New York Times and there was an article titled: “Is There a Doctor on the Plane? Increasingly, Airlines Hope Not”. I’ve always known that there was a company in the background someplace providing support to the flight attendants and pilots on in-flight medical emergencies. Evidently, the major company is MedAire, Inc. which provides services to more than 100 airlines – and, by all accounts very high-quality support. According to their data, only 1.6% of their flights are “diverted” for a landing due to an in-flight medical problem which generally costs about $200,000 – so the emphasis of the airlines is to avoid diversions. Now the diversion results of MedAire are different than the results of a study reported in a 2013 issue of the New England Journal of Medicine which revealed that there was a medical emergency once in every 604 flights and 7.3% led to diversions. The study also reported that 0.3% of medical emergencies on planes end in deaths. The dismaying part of the article was the statement that the airlines “hoped” that no physicians were available on the flight in large measure because in-the-air physicians have a much higher propensity for diverting a plane to land. It got me thinking. What were my results? So, I did a quick tally. Over the last 20 some years, I’ve experienced about 3 – 5 “medical emergencies” with 0 deaths and only 1 diversion – which was for a gent who was having chest pain and all the symptoms of a myocardial infarction. But the vast majority of my clinical experience has been related to in-flight patients who either drank too much the night before or the hours before a flight or, drank too much during the flight. These have been interspersed with “real” medical emergencies like acute asthma due to peanut dust in the air, an apparent appendicitis (although I never did get the final diagnosis), a TIA-like presentation and other assorted “real” experiences. My most challenging was when one of the flight attendants collapsed in the cockpit and I had to work with the crew to extract her from the floor so that they could continue the flight. We made it… Anyway, I decided that zero deaths with one diversion is a record that’s not bad. Hopefully, United will continue to let me fly the (increasingly less) friendly skies. I expect to continue answering the call when I hear, “Is there a doctor on board” or the flight attendant approaches me with a quiet whisper, “Dr. Fickenscher, please come with me right now!”
Politics Before Health Care So That Health Care Trumps Politics – Lancet had a very interesting article several weeks ago entitled, “The world has been warned” by Richard Horton. The essence of the article is that it makes the case for greater involvement by the health care professions in the politics of the day if we are going to be successful in continuing to make the case that investments in health care research and programs make a difference for society. Our focus tends to be on the more immediate questions related to patient care services with strong advocacy for a proper financing and functioning of the health system. Beyond those core areas of focus, the health professions tend to scatter. The article makes the case the we need to listen to the advice of the economist, Dambisa Moyo, Ph.D. who argues in her new book Edge of Chaos (2018) that the support for public investments in health programs and services is weakening. Why? She argues that it all comes back to sustainable economic growth and development – which is not the first order of concern among most health care professionals. Without it; however, the ability of governments to provide the necessary funds for health care programs will wane even though demand is rising. In fact, her central argument is: “politics, and not economics, will be the key driver of human progress and prosperity in years to come”.
In essence, the message is that threats to democracy, factors that diminish economic growth (e.g. growing debt, aging of the populace, natural resource depletion, deepening income disparities and a host of other “economic” considerations are key factors that will be driving the health care debate in future years. We need to listen. The point of the article by Horton is that “Taken together, these pathologies are laying foundations for an unprecedented period of government failure, political instability, social fracture, and community unrest.” You definitely need to read this article and check out Moyo's conclusion that, “liberal democratic capitalism is in retreat”. There are ten prescriptions offered that could help move us back toward a position of stronger support of health care – a core offering of most governments throughout the world. The ten prescriptions have little to do with health care and everything to do with democratic stability. Check it out.
Are We Prepared For Value-Based Care? Short answer, “No!” A new study of over 900 physician organizations by Black Book, a consulting firm, reveals that physician organizations are increasingly concerned about their readiness for the move toward value-based care. Independent and physician-led practices represented 72% of the study group. The essence of the findings; however, was that the groups felt that they were not prepared for a move toward value-based payments. In fact, the study found that 93% of the practices did not have a strategic plan in place "for transforming [to] population health management or value-based care solutions…” My prediction: The coming decade will be littered with also-ran medical groups that failed to prepare for a tsunami of change that is about to sweep the fiscal structure of our health care delivery models. The current system is unsustainable from a purely financial perspective. The Boomers (my generation) will bankrupt the nation if we continue the current course. Change will be led by the states. It already is! Things need to change.
Secondhand Smoke And Marichiwanna – A new study was recently published online in the journal Pediatrics suggesting that the warnings we’ve made about the use of cigarettes in the home by parents should also now be extended to the use of marijuana in the home. The assessment of the study was that “an increase in parents smoking pot around their children could undo decades of effort to protect” children from the effects of secondhand smoke. The homes as risk were those where parents already smoke cigarettes. In those families, the percent of marijuana smokers increased from 11% (2002) to 17% (2015), a notable rise versus those families where cigarette smoking did not exist with an increase of 2% to 4%, respectively. I mean, after all, smoke is smoke…
Healthy Diets = Big Brains – In a new 10-year study from the Netherlands, it was determined that eating a healthy diet like the Mediterranean diet seems to be associated with larger brain volumes. In fact, the brain matter in these individuals had a higher volume of grey and white matter along with a larger hippocampus. The study is consistent with my wife’s missive that I need to eat six cups of fruits and/or vegetables every day, less red meat and less fat (i.e. far less bacon). And, potatoes are not considered a vegetable in her ruling which doesn’t make sense to a farm boy of German heritage unless I decide to become Greek – which she notes is always a good option! But, I’m learning that I should not argue! Besides, now I have a reason – a bigger brain. That and $2.00 will get a Grande dark roast at Starbucks. But, we do seem to be getting consistent results related to the impact of the Mediterranean diet. It’s worth adopting in my estimation.
Sovereignty Of The Tribes Indirectly Challenged – The US Department of Health and Human Services is seemingly stumbling into what could become a decade long litigation nightmare as it continues down the track of requiring Native Americans to hold jobs to keep their health care. The move by HHS directly assaults long held agreements between the US government and the tribes by challenging tribal sovereignty which has been recognized for centuries – not, decades. The Trump Administration has put forward a proposal stipulating that the tribes are a racial group and not separate governments. Needless-to-say, the reaction from the tribes and many members of both parties was quick and negative. In making the preliminary ruling, the feds are passing along the implementation to the states which will no doubt result in a series of inconsistent proposals and approaches toward the tribes. This is not an arcane legalistic argument. Rather, it cuts to the core of agreements made between the US government and the tribal nations over the last two hundred some years. The decision has also split the department where the political appointees have taken a seemingly softer position (i.e. let the states work it out) while the HHS Office of General Counsel have taken a distinctly opposite position (i.e. work requirements apply to everyone and the tribes are not exempt). So, the question is whether the Trumpee discord will be resolved in the Agency or in the courts? HHS political leaders have tried to avoid the controversy by suggesting the matter is a local issue that could be resolved as the federal government and states negotiate the parameters of their proposals. But, duly negotiated agreements between sovereign tribes and the US government would be a difficult thing to undo to say nothing of the political fallout.
Here A Tweet, There A Tweet, Everywhere A Tweet, Tweet – It was only a matter of time before academia caught on to the use and impact of Twitter. In fact, in a recent article, Jason Frank, MD (@drjfrank), a clinician-educator at the Royal College of Physicians and Surgeons of Canada (@RoyalCollege) made a bold statement when he offered this thought: “Within the next decade, you won’t be able to be a successful scholar without having some activity on social media.” Hmmm… Dr. Frank’s thinking is that social media is becoming a ubiquitous tool for sharing one’s scholarship, engaging with the public on the findings of research, advocating for change in public policy and in building new social networks. His contention is that Twitter offers a means for educators, clinicians, and researchers to communicate directly and accelerate information sharing by extending the network from a handful of conference attendees to a worldwide audience of involved researchers. In fact, the data from a recent Pew Research Center study supports the notion that the use of social media is growing substantially among researchers (See graph below). While I’m not going to get in the way of this rapidly moving train, I would like to point out that we need to be highly attuned to the unintended consequences of social media use as it relates to public perception and interpretation of information. My fear is that the nuance of an issue or problem or research finding cannot be effectively conveyed in many – if not most cases – with a string of 140 characters. So, the question for academia is: what are the ground rules for engaging in the use of social media? How should this new communication form be integrated into traditional avenues? And, what types of research needs to be completed to affirm the adopted approach? It’s clear that social media can have a very positive impact on research and the sharing of research results. We need to foster its use and support its deployment. But, let’s also keep a watchful eye on the results…
Percentage of All American Adults and Internet-Using Adults Using at Least One Social Networking Site
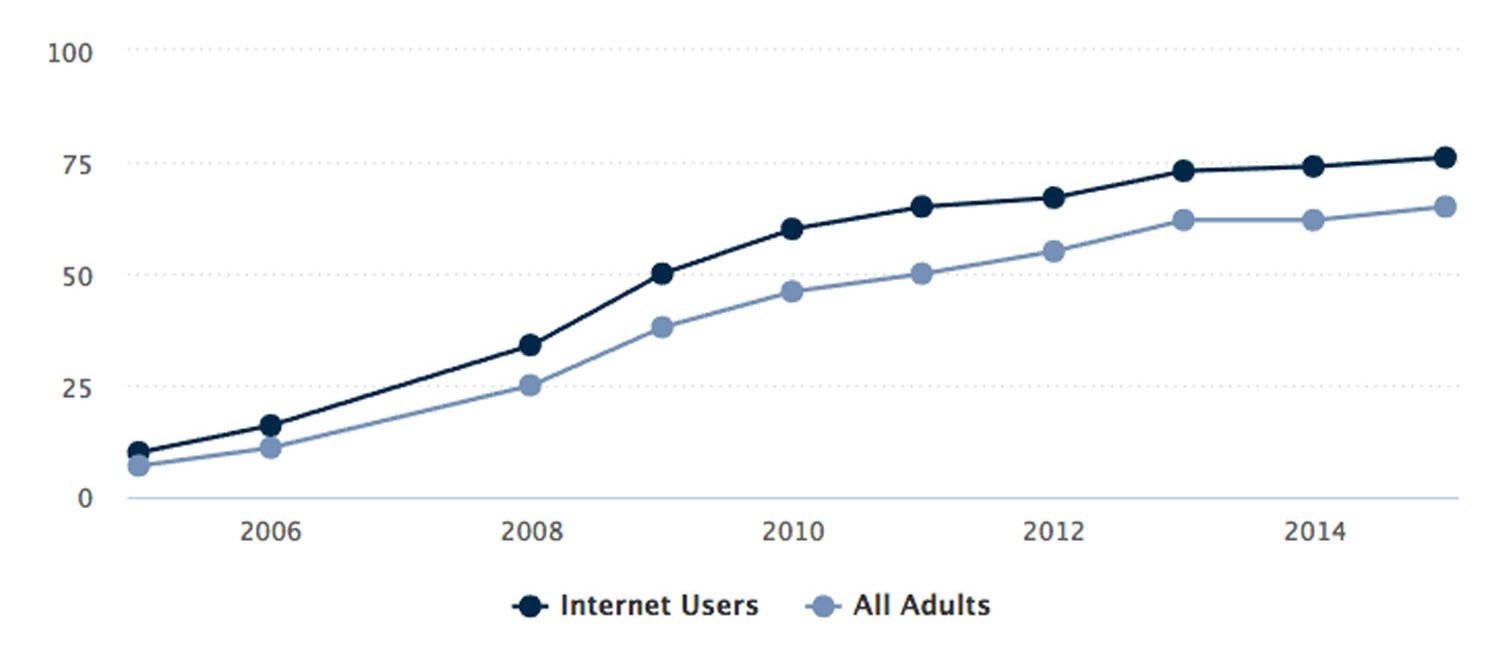
Source: Pew Research Center surveys, 2005-2006, 2008-2015. No data are available for 2007.
Far be it from me that “Dr. Change” would get in the way of “change”. At the same time, I’ve strongly advocated for adapting to rather than resisting change, I’ve also always stated a strong belief that it is incumbent upon those of us who are change agents to monitor what we change since the unintended consequences will sneak up on us over time…
